First person in the world to get the breast cancer vaccine says it’s changed her life. Here’s how it works.
Finding a cure for cancer has been the holy grail in medicine for years. With the exception of the only two cancer vaccines currently available — one for HPV, strains of which can cause cancer, including cervical cancer, and one for hepatitis B, which can cause liver cancer — it’s been elusive.
Now, a breast cancer vaccine, currently in human clinical trials, is aiming to change that.
The vaccine is meant to prevent the recurrence of triple-negative breast cancer, which makes up about 10% to 15% of all breast cancers and is particularly challenging to treat. That’s because the cancer cells in this case don’t have estrogen or progesterone receptors or enough of the protein called HER2 — which is what most effective breast cancer treatments target.
It’s also one of the most aggressive forms of breast cancer since it grows quickly and has a higher rate of recurrence — locally, in the breast area, or to other parts of the body, meaning metastasis. In fact, the risk of the cancer recurring within five years of being diagnosed is nearly three times higher in patients with triple-negative breast cancer than in those who don’t have that type of breast cancer.
How weight loss could be linked to cancerMute
100
So needless to say, a vaccine to prevent recurrence of this type of breast cancer would be a game changer.
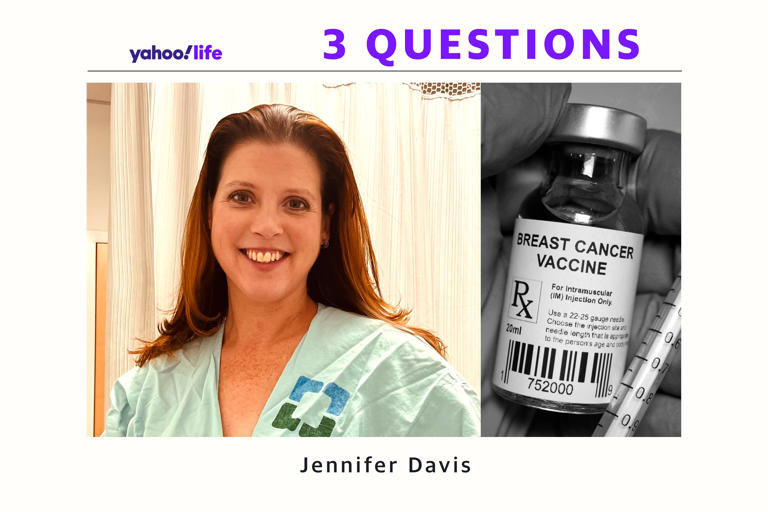
Jennifer Davis, a 46-year-old nurse and mom of three who lives in Ohio, is the first person in the world to receive the vaccine as part of the clinical trial. Here’s why she decided to participate and how the vaccine works.
What made you want to participate in the breast cancer vaccine trial?
For Davis, it’s personal. She was diagnosed with triple-negative breast cancer in September 2018. Her cancer treatment at Cleveland Clinic started soon after that; it involved having a double mastectomy, as well as several rounds of chemotherapy and radiation.
She learned about the breast cancer vaccine trial — 20 years in the making and based on research led by Vincent Tuohy, who died in January 2023 — during a follow-up appointment at Cleveland Clinic. Human trials for the vaccine started in October 2021.
So needless to say, a vaccine to prevent recurrence of this type of breast cancer would be a game changer.
Jennifer Davis, a 46-year-old nurse and mom of three who lives in Ohio, is the first person in the world to receive the vaccine as part of the clinical trial. Here’s why she decided to participate and how the vaccine works.
What made you want to participate in the breast cancer vaccine trial?
For Davis, it’s personal. She was diagnosed with triple-negative breast cancer in September 2018. Her cancer treatment at Cleveland Clinic started soon after that; it involved having a double mastectomy, as well as several rounds of chemotherapy and radiation.
She learned about the breast cancer vaccine trial — 20 years in the making and based on research led by Vincent Tuohy, who died in January 2023 — during a follow-up appointment at Cleveland Clinic. Human trials for the vaccine started in October 2021.
“My [health care] team informed me of the vaccine that Dr. Tuohy had been studying for a long time,” Davis tells Yahoo Life. They told her about the human phase of the trial, which was being conducted right at Cleveland Clinic. “So that was lucky,” she says.
Triple-negative breast cancer is something that “I did not know a lot about when I was diagnosed,” she shares, “but going through everything, you learn so much. It’s just that kind of breast cancer — that particular type — there’s nothing I can take afterward, no tamoxifen [a hormone therapy], and recurrence is high. If it does come back, outcomes are not the greatest. So I wanted to take something — the vaccine was that for me.”
Also, as a nurse, Davis understands that clinical trials are “so important,” adding, “That’s how we advance medicine and make changes and one day, get rid of breast cancer.”
What was it like to be in the clinical trial?
For the trial, which was funded by the Department of Defense, “you couldn’t be more than three years out from your first chemo treatment,” says Davis. “The second guideline was you had to show no signs of recurrence. So there was some testing to go through.”
Once Davis got the OK to participate in the trial, along with 15 other women, she received three injections, each one spaced two weeks apart. “They did lab work prior to every injection,” she says. “I had no side effects except for lumps at the injection site — it was just like any other vaccine or shot that you get.”
Davis, who had two follow-up appointments as part of the trial and still goes to Cleveland Clinic for her checkups, received her last dose of the vaccine in November 2021. So far, the cancer hasn’t come back.
How has getting the vaccine impacted you?
“It’s changed my life,” Davis says. “I don’t think about recurrence every single day.”
That’s significant since, as Davis explains, once you receive a cancer diagnosis like this, it stays with you. “I’m not going to say you don’t ever think about it,” she says. But “the fact that it’s working” — based on Davis’s blood work and immune system response and that the cancer hasn’t returned — “puts your mind at ease as far as recurrence goes.”
She adds: “It’s laid those thoughts to rest. And now I just really live a beautiful life.”
Davis also thinks about what having a vaccine could mean for other women with triple-negative breast cancer — “the fact that it could maybe be eliminated one day,” she says. “I’m happy to be a part of it.”
What experts say
Vaccines are medical tools that harness the body’s immune system to help protect against certain diseases. So it can be a bit confusing that the women who participated in the initial human clinical trials for the vaccine already had triple-negative breast cancer. But, for now, the goal of the vaccine is to prevent that same cancer — which, again, has a high recurrence rate — from coming back.
Amit Kumar, chairman and chief executive officer of Anixa Biosciences, which is licensed to create the vaccine being tested by Cleveland Clinic, says that 42% of women with triple-negative breast cancer will get the cancer again within five years. “It’s typically much more aggressive, so the outcome for those women is not very good,” he tells Yahoo Life. The purpose of the breast cancer vaccine is to “eliminate the recurrence for those women and eventually, prevent the cancer from ever arising.”
While the focus right now is on triple-negative cancer because “it’s the most lethal form,” says Kumar, “we eventually want to do clinical trials in other types of breast cancer. We might be able to eliminate breast cancer as a disease, just as we have eliminated polio [in the U.S.] and smallpox.”
How does the breast cancer vaccine work?
The vaccine works by training the immune system to recognize alpha-lactalbumin, a beneficial protein normally found in human milk, explains Justin Johnson, program manager at Cleveland Clinic Lerner Research Institute. “In healthy tissues, alpha-lactalbumin is only made in the breast and only during lactation,” he tells Yahoo Life. “However, breast tumors often also express alpha-lactalbumin, particularly in the case of triple-negative breast cancer.”
As Kumar puts it: “If a woman isn’t lactating, the only time that protein shows up is cancer.”
Johnson explains that the vaccine helps the immune system “identify and attack” the emerging cancer cells by targeting this protein. “In women of post-childbearing years, the vaccine may provide safe and effective protection against breast cancer as soon as it begins to develop,” he says.
How promising are the results so far?
The phase I clinical trial began at Cleveland Clinic two years ago, and “to date, we have immunized 16 women, all of whom are TNBC survivors, with the breast cancer vaccine,” Johnson says. “The side effects have generally been mild, consisting mainly of irritation at the injection sites. Our data so far shows that we have generated robust immunity to the alpha-lactalbumin target in the majority of the subjects, even at the lowest dose tested.”
Johnson adds that while a successful immune response is critical to establishing protection against tumors, “we do not yet know if the vaccine will be clinically effective. We plan to monitor the subjects long-term for breast cancer recurrence.”
Dr. G. Thomas Budd, of Cleveland Clinic’s Taussig Cancer Institute and principal investigator of the study, said in a statement: “The ultimate goal of this research trial is to develop a vaccine that could prevent breast cancer in people who are at risk. It’s a lofty goal, but that would be what we would hope for. There are a lot of steps to go through before that. This may not work, but you know it’s one of those journeys of 1,000 steps that has to start. So we’re taking the first steps.”
If larger clinical trials do well — phase II is up next and scientists want a diverse group of patients to participate — Kumar thinks the vaccine could be available within five years “for women like Jenni [Davis] who have already had cancer and are worried about recurrence.”
But, he points out, the vaccine is still in its early stages of human testing. “We want to do the proper studies and make sure that it’s safe,” he says. “You’ve got to make sure there are an incredibly small number of side effects.”
Still, it’s hard for people like Kumar and Davis not to think about what it would mean to have an effective breast cancer vaccine available. “If we could just have women get three shots and eliminate cancer — triple-negative cancer and eventually breast cancer — that would be amazing,” says Kumar. “It would also change the way cancer research is done.”
